Stay Current in Pediatric Surgery
Podcast door StayCurrent: Pediatric Surgery
Tijdelijke aanbieding
2 maanden voor € 1
Daarna € 9,99 / maandElk moment opzegbaar.
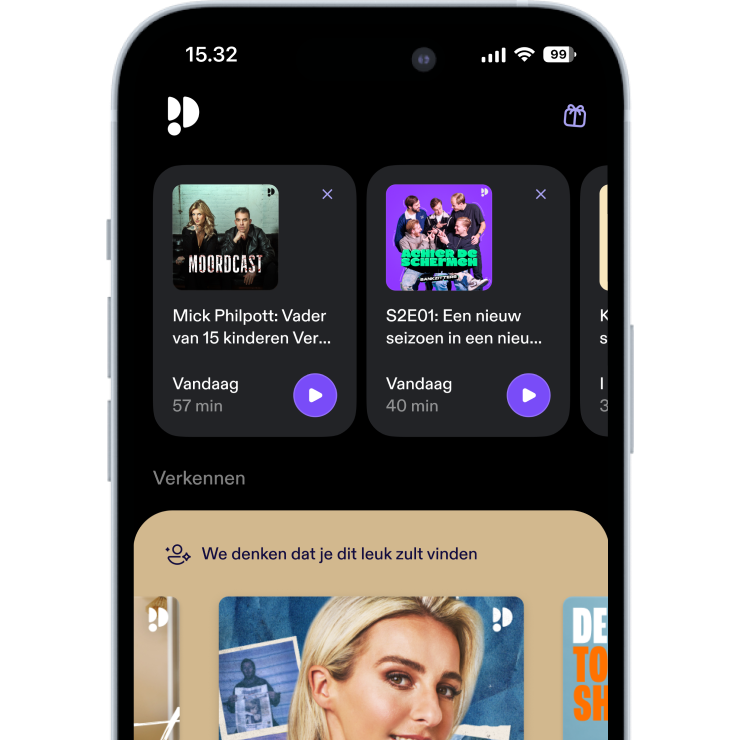
Meer dan 1 miljoen luisteraars
Je zult van Podimo houden en je bent niet de enige
4.7 sterren in de App Store
Over Stay Current in Pediatric Surgery
Through GlobalCastMD’s world-class network of physicians and technology, any health system can provide their doctors access to ongoing mentoring and education. Companies can leverage this same network to more effectively train physicians on products and use it to help train their own sales force. Our educational materials aim to provide entertaining, interactive education for anyone, regardless of geography. We truly are: Dedicated to the rapid advancement of care. Everywhere.
Alle afleveringen
418 afleveringenIn this session from the 12th Annual Update Course in Pediatric Surgery, Dr. Bhargava Mullapudi (Children’s Mercy Kansas City) presents updated strategies in Wilms tumor management, exploring how tumor biology and global guidelines are shaping decisions on surgery vs chemotherapy first. Key Highlights: * COG vs SIOP Guidelines: North American centers (COG) typically favor primary surgery, while European protocols (SIOP) begin with chemotherapy—highlighting major global practice differences. * Impact of Tumor Genetics: Loss of heterozygosity (LOH) at chromosomes 1p and 16q, as well as gain of 1q, influence chemotherapy decisions even in lower-stage disease. * Staging and Size Aren’t Enough: While age and tumor weight are considered, biological markers ultimately guide treatment, challenging simplified “under 2 years / under 550g” rules. * Shifting Practice Patterns: Even for Stage I tumors, presence of LOH may justify adding chemotherapy, depending on evolving Children’s Oncology Group recommendations. * Pathology-Informed Protocols: Surgeons must often pause for biological profiling before placing ports or initiating adjuvant therapy. This presentation underscores the importance of precision medicine in Wilms tumor care—and how treatment pathways increasingly rely on molecular markers, not just stage and weight.
In this session from the 12th Annual Update Course in Pediatric Surgery, Drs. Rebecca Stark and Steven Lee from Seattle Children’s Hospital walk through the timing, technique, and evolving protocols for performing ECMO and surgical repair in cases of severe congenital diaphragmatic hernia (CDH). Key Highlights: * VA ECMO with bivalirudin: The presenters advocate for bivalirudin as a preferred anticoagulant over heparin due to its short half-life, predictable response, and ease of control—making it ideal for ECMO patients requiring surgery. * Dilute thrombin time for monitoring: They highlight a lab-friendly technique for monitoring bivalirudin using dilute thrombin time—5x more specific and sensitive than PTT and easily implementable in any lab. * Safe and timely surgical repair on ECMO: Early CDH repair (within 8–24 hours of ECMO initiation) can be performed with minimal bleeding and less tissue edema when using bivalirudin and meticulous technique. * Institutional buy-in for early repair: The team underscores the importance of cross-disciplinary collaboration—including neonatologists, anesthesiologists, and weekend OR availability—to enable early ECMO repair protocols. * Risk-stratified vs early repair strategy: Some centers risk-stratify ECMO patients, but Stark and Lee favor universal early repair to avoid complications associated with delayed surgery in non-weanable patients. * Evolving national practices: As of this year, over 80% of CDH Study Group centers are now performing early repair on ECMO—showing how rapidly clinical protocols can shift with strong supporting data. This session emphasizes the role of proactive planning, team-based decision-making, and flexible protocol development in improving outcomes for neonates with severe CDH requiring ECMO.
In this session from the 12th Annual Update Course in Pediatric Surgery, Dr. Margaret Mutch from Australia walks through the complexities of chest wall reconstruction following thoracic osteosarcoma resection in a pediatric patient. Key Highlights: * Massive resection and reconstruction: A 14-year-old patient underwent an aggressive en bloc resection involving ribs 4–7 and vertebral bodies T4–T7. The team used a combination of resorbable molded plates, Permacol mesh, and Gore-Tex patches to stabilize and recreate the chest wall structure. * Soft tissue closure with latissimus flap: A latissimus dorsi flap was mobilized for robust coverage, reducing dead space and supporting tissue healing over the reconstructed area. * Use of ROLL technique for lymph node excision: The team employed radio-guided occult lesion localization (ROLL) using Technetium-99 to precisely identify and remove targeted lymph nodes. * Managing early complications: Postoperative challenges included sterile seromas, a wound infection, and mild scoliosis—all managed conservatively with good outcomes. * Addressing recurrence and reoperation: When local recurrence occurred 18 months later, a second reconstruction involving the sternum and cement mesh was required, illustrating the long-term complexity of these cases. * Future outlook for pediatric reconstructions: Dr. Mutch emphasized the lack of standardization in pediatric materials and techniques, pointing toward a future where custom 3D-printed implants and biologics may offer better long-term solutions. This session highlights the surgical precision, interdisciplinary coordination, and resilience required to manage large-scale reconstructions in growing children—where both oncologic control and functional outcomes must be balanced.
We are back with another episode of our Journal of Pediatric Surgery article review podcast. This time we have three publications from the second quarter of 2025, April, May and June issues. This time we're talking to editors Drs. George Holcomb III, Alana Beres and Shaun Kunisaki joined by authors Drs. Eric Skarsgard, Amanpreet Brar, Anoosha Moturu and Derek Wakeman. Host: Em Gootee, MD Articles: https://pubmed.ncbi.nlm.nih.gov/39826297/ [https://pubmed.ncbi.nlm.nih.gov/39826297/] Shieh HF, Jennings RW, Hamilton TE, Izadi S, Zendejas B, Smithers CJ. Tracheobronchopexy to Avoid Tracheostomy in Esophageal Atresia Patients With Severe Life-Threatening Tracheobronchomalacia. J Pediatr Surg. 2025 Apr;60(4):162152. doi: 10.1016/j.jpedsurg.2024.162152. Epub 2025 Jan 3. PMID: 39826297. https://pubmed.ncbi.nlm.nih.gov/39865003/ [https://pubmed.ncbi.nlm.nih.gov/39865003/] Brar A, Gow KW, Skarsgard ED. Pediatric Surgical Outreach: An Underutilized Resource for Increasing Children's Surgical Capacity in Canada. J Pediatr Surg. 2025 May;60(5):162174. doi: 10.1016/j.jpedsurg.2025.162174. Epub 2025 Jan 19. PMID: 39865003. https://pubmed.ncbi.nlm.nih.gov/39743432/ [https://pubmed.ncbi.nlm.nih.gov/39743432/] Moturu A, Coleman M, Mets C, Thompson V, Grant C, Ko CY, Saito JM, Berman L, Wakeman D. Identifying Quality Improvement Targets After Pediatric Gastrostomy Tube Insertion: A NSQIP-Pediatric Pilot Study. J Pediatr Surg. 2025 Jun;60(6):162107. doi: 10.1016/j.jpedsurg.2024.162107. Epub 2024 Dec 17. PMID: 39743432.
In this session from the 12th Annual Update Course in Pediatric Surgery, Drs. Rebecca Stark and Steven Lee from Seattle Children’s Hospital walk through the timing, technique, and controversies surrounding ECMO in severe congenital diaphragmatic hernia (CDH) cases. Key Highlights: * VV vs VA ECMO: While venovenous (VV) ECMO is gaining traction with improved cannulas, venoarterial (VA) ECMO remains the predominant choice for most centers treating CDH. * When to initiate ECMO: Early intervention is often favored in high-risk CDH cases, especially when prenatal imaging suggests severe compromise. * SPHERE protocol in decision-making: A structured approach from Michigan offers criteria for ECMO vs comfort care, but outcome prediction remains unreliable—50% of decisions based on early data may be incorrect. * Controversy in selection: Dr. Stark advocates for offering ECMO to all infants with isolated unilateral CDH, emphasizing the importance of treating every case as a potential survivor. * Role of prenatal counseling: Early, transparent discussions with families are critical for navigating high-stakes decisions and aligning on care pathways. This session underscores both the technical and ethical complexity in managing severe CDH—and the need for thoughtful protocols paired with clinical flexibility.
4.7 sterren in de App Store
Tijdelijke aanbieding
2 maanden voor € 1
Daarna € 9,99 / maandElk moment opzegbaar.
Exclusieve podcasts
Advertentievrij
Gratis podcasts
Luisterboeken
20 uur / maand